NAIROBI, Kenya, Jan 20 – New estimates reveal that at least 1.27 million deaths per year are directly attributable to antimicrobial resistance (AMR).
Globally, AMR ranked highest with Sub-Saharan Africa being the most affected region.
A Global Burden of Disease study, published in the Lancet, a peer-reviewed general medical journal, based on estimates across 204 countries and territories, revealed that AMR had become a leading cause of deaths globally higher than HIV/AIDS or Malaria.
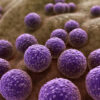
AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines, making infections harder to treat and increasing the risk of disease spread, severe illness and death.
In Sub-Saharan Africa, over 255,000 people died as a direct result of AMR in a single year – around half of these were children under the age of 5 and a particularly high number from vaccine preventable pneumococcal bacterial disease.
“Common infections such as lower respiratory tract infections, bloodstream infections, and intra-abdominal infections are now killing hundreds of thousands of people every year because bacteria have become resistant to treatment. This includes historically treatable illnesses, such as pneumonia, hospital-acquired infections, and food borne ailments,” the data showed.
In 2019, 129,000 deaths attributable to AMR in Sub-Saharan Africa were in children under the age of 5.
This includes a high number of infections from E. coli, usually acquired through contaminated food and water.
Highlighting the need for greater action to tackle the problem of AMR, Dr Mirfin Mpundu, Director of ReAct Africa, challenged stakeholders in the health sector to formulate an action plan to address the challenge.
“Momentum that the global community built following the AMR Global Action Plan in 2015 has slowed down and there has not been a proportionate response to the gravity of the problem.”
Poorer countries are worst affected but antimicrobial resistance threatens everyone’s health, the report noted.
Urgent investment in new drugs and using current ones more wisely are recommended to protect against it.
The overuse of antibiotics in recent years for trivial infections means they are becoming less effective against serious infections undermining their ability to carry out essential medical practice safely, including surgery, childbirth and cancer treatment since infection is a risk following these procedures.
Past projections estimated that as many as 10 million annual deaths from AMR could occur by 2050.
Dr Ramanan Laxminarayan, from the Centre for Disease Dynamics, Economics and Policy, said much of the world faced the challenge of poor access to affordable, effective antibiotics – and that needed to be taken seriously by political and health leaders everywhere.
While progress has been made, the necessary funding and capacity to implement such plans are often falling behind, with COVID-19 further disrupting the global health agenda.
“AMR is threatening the ability of clinicians to keep patients safe from infections and undermining their ability to carry out essential medical practice safely, including surgery, childbirth and cancer treatment since infection is a risk following these procedures,” the data showed.
Whilst all seven of the leading bacteria have been identified as ‘priority pathogens’ by the World Health Organization (WHO) only two have been a focus of major global health intervention programmes – S. pneumoniae (primarily through pneumococcal vaccination) and M. tuberculosis.
The report provided immediate actions that can help countries around the world protect their health systems against the threat of AMR which includes the need to take greater action to monitor and control infections, globally, nationally and within individual hospitals.
In December, WHO through the support of Saudi Arabia identified seven countries to benefit from an initial comprehensive technical package to support the implementation of national action plans on AMR based on the specific country needs.
These countries included Egypt, Ethiopia, Jordan, Indonesia, Nigeria, Pakistan and Sudan.