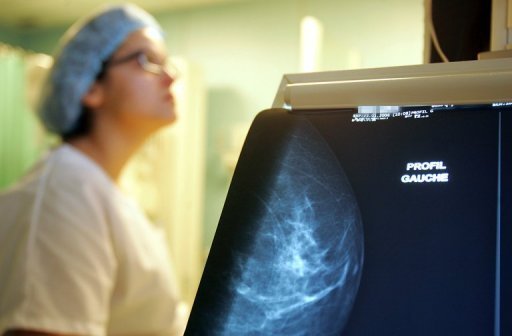
Women diagnosed with cancer in one breast often face a difficult decision of whether to surgically remove both, and a study Wednesday found double mastectomies may be performed too often.
The surgery does not increase survival in most women, and is typically recommended for about 10 percent of women considered at high risk for breast cancer.
Some 69 percent of women who underwent surgery to remove a healthy breast did not have major family or genetic risk factors, said the study in the Journal of the American Medical Association.
Meanwhile, just a quarter of women who did face a higher risk of future cancer had the recommended surgery to remove both breasts, known as a contralateral prophylactic mastectomy.
Women with certain mutations in the BRCA1 and BRCA2 genes, or who have a strong family history of breast cancer are usually counseled to have both breasts removed after a diagnosis in one, to avoid a recurrence.
“Women appear to be using worry over cancer recurrence to choose contralateral prophylactic mastectomy,” said lead author Sarah Hawley, associate professor of internal medicine at the University of Michigan Medical School.
“This does not make sense, because having a non-affected breast removed will not reduce the risk of recurrence in the affected breast,” Hawley said.
The research was based on a sample of 1,447 US women, average age 59, who were diagnosed with stage 1-3 cancer in one breast.
Nearly eight percent of the women had both breasts removed, 35 percent had just the affected breast removed, and nearly 58 percent had breast conservation surgery, in which only the lump is taken out.
Researchers found that women with higher education levels were more likely to choose contralateral prophylactic mastectomy, with concern about the disease surfacing in the healthy breast listed as a main factor in their decision.
These women could be driving a rise in double mastectomy surgeries over the past decade, even though the procedure carries an increased risk of surgical complications and a longer recovery time, researchers said.
Hawley and colleagues noted that their data was based on information obtained from surveys in Los Angeles and Detroit, and may not be generalizable to all areas.
In addition, the information was based on patients’ self-reports, and inaccurate recall of genetic testing and results could have skewed the figures, they said.
An accompanying editorial by Shoshana Rosenberg and Ann Partridge of the Dana-Farber Cancer Institute in Boston, pointed out the emotional complexities that women face after receiving a diagnosis of breast cancer.
“Anxiety and fear certainly hamper optimal decision making,” they wrote.
“While CPM might be considered overtreating women without clinical indications, it might still be the right choice for some women for risk reduction, cosmetic, and/or emotional reasons.”
They urged doctors to share the decision-making process with patients in order to find “balance around this issue.”
